Coaching to Competence
As part of Competence by Design (CBD), there is an important role for coaching in resident learning and progression. It takes skill to coach someone effectively, which is why a group of clinician educators have developed the “Coaching to Competence” online learning modules.
The CBD Coaching Model uses assessment as a learning tool, not just an evaluation method. Coaching in the Moment is part of the model that links to RX-OCR step-by-step process. It requires clinicians to establish Rapport and set eXpectations with their residents, Observe the residents doing their daily work, provide Coaching feedback, and Record the encounter.
“Coaching to Competence” consists of five interactive activities that allow anyone who teaches residents to practice applying the RX-OCR coaching process. The activities are meant to help you identify gaps in skills and knowledge related to coaching.
CPD Credits
This activity is an Accredited Self-Assessment Program (Section 3) as defined by the Maintenance of Certification Program of the Royal College of Physicians and Surgeons of Canada, and approved by the Royal College Continuing Professional Development Unit. You may claim a maximum of 30 minutes for each module (credits are automatically calculated).
Access Details
For more information visit the Royal College of Physicians and Surgeons of Canada website: http://www.royalcollege.ca/mssites/rxocr/en/story_html5.html
Webinar Recordings: Ergonomics and Mindfulness in the Operating Room. Providing Care to Your Patients While Avoiding Becoming One
The Canadian Ophthalmological Society is pleased to provide you to a recording of the webinar on practical ergonomic tips in the ophthalmology operating room, that took place on December 9, 2019.
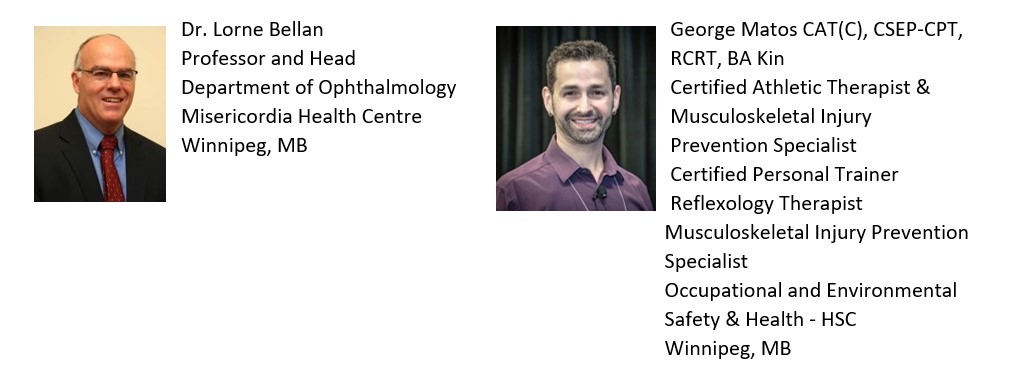
In the session George Matos, Musculoskeletal Injury Prevention Specialist and ophthalmologist Dr. Lorne Bellan review how to adapt your posture to protect yourself through a day of surgery. This webinar includes thoughts to have in mind at the start of your surgical day, including how to set up your foot pedals, chair, operating table and surgical microscope, each to optimize your posture and support during your day of surgery and to minimize the risk of repetitive stress injuries.
Learning Objectives
At the end of this webinar, participants will be able to:
- Describe optimal posture for a day of cataract surgery
- Position foot pedals optimally from an ergonomics perspective
- Set up your surgical chair for optimal arm, leg and back support
- Set the microscope position and angle optimally for your neck
- Re-introduce equipment/movement patterns to lessen musculoskeletal strain that can be overlooked
CPD Credits
This webinar archive is an Accredited Group Learning Activity (Section 1) as defined by the Maintenance of Certification Program of the Royal College of Physicians and Surgeons of Canada, and was approved by the Canadian Ophthalmological Society. You may claim a maximum of 1 hour.
Access Details
To access the archived (recorded) version of the webinar visit the event website: https://event.on24.com/wcc/r/2140596/980B5EE498FA3BA26DF28AC29830E995
This program was delivered with financial support from an educational grant from provided to the COS by the Canadian Medical Association, MD Financial Management and Scotiabank.
Musculoskeletal Disorders in Ophthalmologists
Did you know?
Work-related musculoskeletal disorders in ophthalmologists are high, ranging from 51-80% across studies.
This module was developed to showcase best ergonomic practices and injury prevention. View the module, online through the Queen’s University website.
Learning Objectives
- Review the importance of ergonomics for ophthalmologists
- Identify areas in the clinic and operating room that may predispose to musculoskeletal disorders
- Learn proper ergonomic risk factor modification
- Recognize signs and symptoms of musculoskeletal disorders, understanding the importance of early intervention
CPD Credits
Completion of this 30 minute online learning module has been determined by Queen’s University to be eligible for 0.50 hours of Royal College of Physicians and Surgeons of Canada Section 2: Self Learning for Specialists credits.
For more information visit the Queen’s University website.

Happy People Work Better
The Canadian Journal of Physician Leadership (CJPL) is a peer-reviewed journal launched in 2014. Published quarterly, it focuses on topics and issues related to leadership and the health care system as they pertain mainly, but not exclusively, to physicians and physician leaders.
Volume 4, Issue number 3, Happy People Work Better features:
- Achieving Joy in Canada’ health care system: What can we do today?
– Johny Van Aerde, MD, PhD - Turning burnout into joy
– Mamta Gautam, MD - Transforming health care through systems and stories
– Cheryl Heykoop, DSocSci, and Guy Nasmyth, PhD - Five fundamentals of civility for physicians: Part 2
– Michael Kaufmann, MD - The continuing challenge of patient-centred care
– Michael Gardam, MD and Judith John, BA - Could Saskatchewan become the best place in the world to practise medicine?
– Susan Shaw, MD, and Ivan Muzychka - Accountability and trust: Sitting on a three-legged stool
– Darren Larsen, MD - Physician leadership development through the lens of LEADS and competency-based education
– Ming-Ka Chan, MD, Celia Rodd, MD, Elisabete Doyle, MD, Eleanor MacDougall, MD, Jenette Hayward, MD, and Karen Gripp, MD - Stories from our CCPES: Journey into the unknown
– Gary Ing, MD - Stories from our CCPES: My leadership journey
– William Sischek, MD
CMA Policy on Physician Health
This policy provides a series of broad, aspirational recommendations to help guide stakeholders at all levels of the health system to promote a healthy, vibrant, and engaged profession.
For more details visit the Canadian Medical Association website.

U of T Med: Heal Thyself
U of T Med is an alumni magazine like no other. Bold, ambitious and lively, we dive into medicine’s most pressing topics. Heal Thyself is the U of T Med publication from Summer 2017 addressing the topic of physician mental health.
This issue features:
- Can We Talk About Physician Mental Health?
- Who Heals the Healer?
- The Unspeakable Struggle
- A Heavy Toll
- Under Pressure
- After the Tragedy
- The Millennial Approach
- Ready, Steady, Reset
- Human Beings First and Foremost
- Unvarnished Truth
To review the U of T Med Summer 2017 issue, visit the website.
Earning and Claiming CPD credits via the CJO
Earning CPD credits
You can earn Section 2 credits toward your Royal College of Physicians and Surgeons of Canada (RCPSC) Maintenance of Certification (MOC) requirements by:
- Reading CJO articles: each journal article that you read and deem has had a significant impact on your learning or practice can be recorded individually — you will receive one (1) credit per article.
- Peer reviewing CJO articles: you can earn up to 15 credits per year as a Peer Assessment activity. The 15 credits are eligible for your yearly contributions.
Claiming CPD credits
To claim CPD credits for reading CJO articles, you must record them in your MAINPORT ePortfolio as Section 2 Self Learning credits.
To claim CPD credits for peer reviewing CJO articles, you can either record them in MAINPORT yourself, or you can opt into our automatic transfer program and we will submit your Section 2 Peer Assessment credits directly to the RCPSC every year. The credits will appear in your MAINPRO dashboard for your review and approval. To opt into this program, please contact the Managing Editor at [email protected].
Why Organizations, Researchers, and Patients Are Falling Prey to Predatory Journals
Participate by Live Stream or in-person on October 10 from 1:30 – 2:30 PM. This interactive talk will provide an overview of what predatory journals are and describe how they are having an impact on organizations, researchers, and patients. In doing so, the talk will touch on related topics including academic incentives, research funding, and science policy. It will discuss the impact of predatory journals on knowledge synthesis efforts and health literacy. It will recommend safeguards that stakeholders can put in place to limit interaction with these journals and to help reduce waste in how biomedical research is shared and used.
The speaker, Dr. Kelly Cobey, is an Investigator at the Ottawa Hospital Research Institute (OHRI) working in the Centre for Journalology.
CPD Credits
Earn 0.5 MOC credits under Section 2 for participating.
Access Details
For more information and to register visit the CADTH website.
“Little” things make BIG differences: Recognizing and Managing Disruptive Behaviour in the Clinical Environment
“Little” things make BIG differences is an online module, and has been accredited as a Section 3: Self-Assessment Program.
The program designed to help practicing physicians, residents, administrators, and other team members build knowledge, skills, and attitudes required to better recognize and manage issues of disruptive behavior in their team based settings.
Premise of the Program
The program follows the case of Mrs. Wendy Lee, a patient who needs surgery at the Pondview Health Network.
Mrs. Lee’s surgery did not go as planned and Dr. Gin Staples, an administrator at the hospital, needs to review the case in order to make recommendations. Your objective is to review Mrs. Lee’s case from the perspective of the team members and patient in order to help Dr. Staples develop recommendations that foster “just culture” at the Pondview Health Network.
As you read through the case you are presented with questions. Record your answers for each question as you go through. There is an answer key at the end of this page to help you gauge your understanding of the content. Answering these questions helps you to compile findings that inform final recommendations for Dr. Staples and can also be used as part of a Personal Learning Project to earn Section 2 MOC credits.
Learning Objectives
Upon the completion of this simulation-based learning activity, you will be able to:
- Recognize the environmental stimuli that can precipitate disruptive behaviour
- Identify strategies for mitigating disruptive behaviour in the clinical environment
- Describe the impact disruptive behaviour has on the clinical environment
- Apply prescribed techniques that promote a “just culture” in the clinical environment
- Reflect on experiences with disruptive behaviour in the clinical environment
CPD Credits
“Little” things make BIG differences is an Accredited Self-Assessment Program (Section 3) as defined by the Maintenance of Certification Program of the Royal College of Physicians and Surgeons of Canada, and approved by Royal College Continuing Professional Development Unit. You may claim a maximum of 2 hours (credits are automatically calculated).
Access Details
To access the module please visit the Royal College of Physicians and Surgeons of Canada website.



