CJO January 2025: Featured Highlights on Glaucoma
The following CJO Highlight summarizes key findings from the journal article “Acute Angle-Closure Glaucoma Risk: A Comparative Study of Escitalopram and Antidepressants.”1
Acute angle-closure glaucoma (AACG) is an ophthalmic emergency that has been linked to selective serotonin reuptake inhibitors (SSRIs) due to their mild anticholinergic effect and possibility of mydriasis. Escitalopram, one of the most prescribed SSRIs, has been implicated in the risk of AACG in case reports. However, prior to this CJO study by Khan et al., it remained unclear whether AACG secondary to escitalopram is a class effect or carries a higher risk than other SSRIs. The highlighted study investigated whether escitalopram poses a greater risk of AACG compared to other SSRIs or non-SSRI antidepressants. A total of 865,546 subjects were included to assess the incidence of AACG among new users of citalopram, escitalopram, sertraline, and venlafaxine. Results indicated trends toward a lower AACG risk in users of citalopram, escitalopram, and venlafaxine compared with sertraline, though none of these differences reached statistical significance. Findings suggest that escitalopram may be associated with a reduced risk of AACG, but further research with larger cohorts is needed. Clinicians should remain cautious when prescribing antidepressants, particularly for patients at risk of glaucoma.
To access the full article, please follow the link below:
Reference:
- Khan HM, Schendel S, Mikelberg FS, Etminan M. Acute angle-closure glaucoma risk: a comparative study of escitalopram and antidepressants. Can J Ophthalmol. 2025 Jan 24:S0008-4182(25)00004-3. doi: 10.1016/j.jcjo.2025.01.004. Epub ahead of print. PMID: 39870359.
Submitted by: Audrey-Anne Lapierre
Reviewed and Approved by: Anne Xuan-Lan Nguyen, MD
COS Forum 2025: Eyes on Tomorrow

This webinar took place on January 23, at 7:00 PM EST. If you missed it, not to worry! A recording is now available at the bottom of this page.
Hear from speakers on key topics, including: Advocacy in Eye Health Barriers, Corneal Donation, Ergonomics and Injury Prevention, Ethical Considerations in Ophthalmology, and Annual Meeting Updates: 2025 AI Stream Preview.
After this session, participants will:
- Understand how COS is advocating for policy changes at the government level to improve eye care accessibility and quality.
- Be more aware of the latest information on ergonomics and injury prevention and how the profession is affected by injury. Present the latest updates on funding opportunities to CMA and outputs related to project development.
- Know more of the status of the COS Annual Meeting in 2025 and provide information about our new stream on Artificial Intelligence.
- Understand the importance of ethics in our profession and learn about the virtues exemplified by the ethical physician.

Join Dr. Nina Ahuja, Chair of the Council on Advocacy for the Canadian Ophthalmological Society, as she explores the multifaceted role of advocacy in ophthalmology. Discover how advocacy shapes clinical practice, drives research, raises public awareness, and influences health policy. Learn actionable strategies to amplify our collective voice, inspire meaningful change, and ensure a future of eye care defined by inclusivity, innovation, and excellence.
*Elisabeth Fowler covers this topic in our French Forum on January 29.

Dr. Adam Muzychuk shares exciting updates on the planning process and highlights of what to expect at the 2025 COS Annual Meeting in Vancouver. As the COS Annual Meeting Chair and a new member of the COS Board, Dr. Muzychuk discusses how the event is shaping up to be an extraordinary experience for Canadian ophthalmologists, featuring world-renowned experts across every subspecialty.
*Dr. Mona Dagher covers this topic in our French Forum on January 29.

Dr. Samir Jabbour delves into current guidelines on corneal donation and their impact on the Canadian eye banking system. His presentation will address the specific limitations faced by corneal donors from the MSM community and explore future opportunities to improve these regulations.

Dr. Chryssa McAlister runs a diverse comprehensive ophthalmology practice with an academic focus on bioethics and organizes the biennial Macrae Bioethics and Professionalism Course for senior ophthalmology residents. McAlister is a frequent speaker at conferences on topics of bioethics in ophthalmology and medical education. Her presentation will highlight how to cultivate virtues in a business model of ophthalmology.

Dr. R. Rishi Gupta is on a mission to educate every Canadian Ophthalmologist on injury prevention and ergonomics. His presentation will highlight the strong collaboration and efforts of the newly established COS working group, and their lofty goals for the years to come. Not to worry – we’ve got your back!
*Dr. Cyril Archambault covers this topic in our French Forum on January 29.

Our COS President, Dr. Mona Dagher, will be moderating the session.
Understanding Uveal Melanoma: A Rare but Serious Eye Cancer
Submitted by: Joshua Huang
Reviewed and approved by: Dr. Marie-Josée Aubin, Dr. Anne Xuan-Lan Nguyen
What is Uveal Melanoma?
Uveal melanoma (commonly referred to as ‘intraocular melanoma’) encompasses melanomas that arise in the iris, ciliary body, and choroid, all of which make up the uvea or uveal tract. The uvea is the second most common location for the development of melanoma, after the skin, and uveal melanoma is the most common primary intraocular cancer in adults. Although it is rare (it affects 5 adults out of 1 million people each year), it can lead to vision loss, eye loss and even death.
Symptoms
Although most patients are asymptomatic, symptoms can include:
- Blurry vision
- Flashes or photopsia
- Floaters or spots in your vision
- Visual field loss
- Visible dark spot on your iris
- Pain (uncommon)
Risk Factors
- Older individuals (peak age of 70)
- Existing skin moles,iris or choroidal nevi
- Fair skin and light eye colour
- Skin that burns easily with an inability to tan
- Arc welding
- Indoor suntan bed use
- Note: Although sunlight is a risk factor for cancers of the skin and the ocular surface, its association with uveal melanoma is controversial and has not been established
Diagnosis
- Complete eye examination, including a dilated view of the back of the eye (fundus)
- Ocular ultrasonography (B-scan)
Treatment Options
- Based on size and location
- Includes observation, resection, radiation therapy, or enucleation
- Immunotherapy if the cancer has spread (metastasis)
Conclusion
Despite advancing uveal melanoma treatment modalities, there has been no change in survival over the last 50 years. Therefore, awareness and prevention are critical to improving outcomes. talk to your doctor or eye care provider for a complete annual eye exam.
2025 EPSAA Scientific Meeting
The Eye Physicians and Surgeons Association of Alberta is proud to announce that the 2025 Scientific Meeting and AGM is scheduled to take place from February 7th to February 8th, 2025 in Banff, Alberta.
From this program, learners are expected to:
- Discuss modern approaches to diabetic retinopathy;
- Build knowledge of contemporary neuro-ophthalmic diagnoses;
- Evaluate approaches to glaucoma care;
- Build knowledge of clinical presentations and risk factors for visual loss due to systemic medications;
- Update knowledge on novel research being performed by resident physicians in Alberta.
The 2025 Eye Physicians and Surgeons of Alberta Annual Scientific Meeting is an Accredited Group Learning Activity (Section 1), as defined by the Maintenance of Certification Program of The Royal College of Physicians and Surgeons of Canada and was approved by the Canadian Ophthalmological Society. Physicians may claim a maximum of 5.5 hours.
More program details are included in the PDF below. For more information on registration, click HERE.
Whistler Cataract and Retina Update: Innovations and Insights
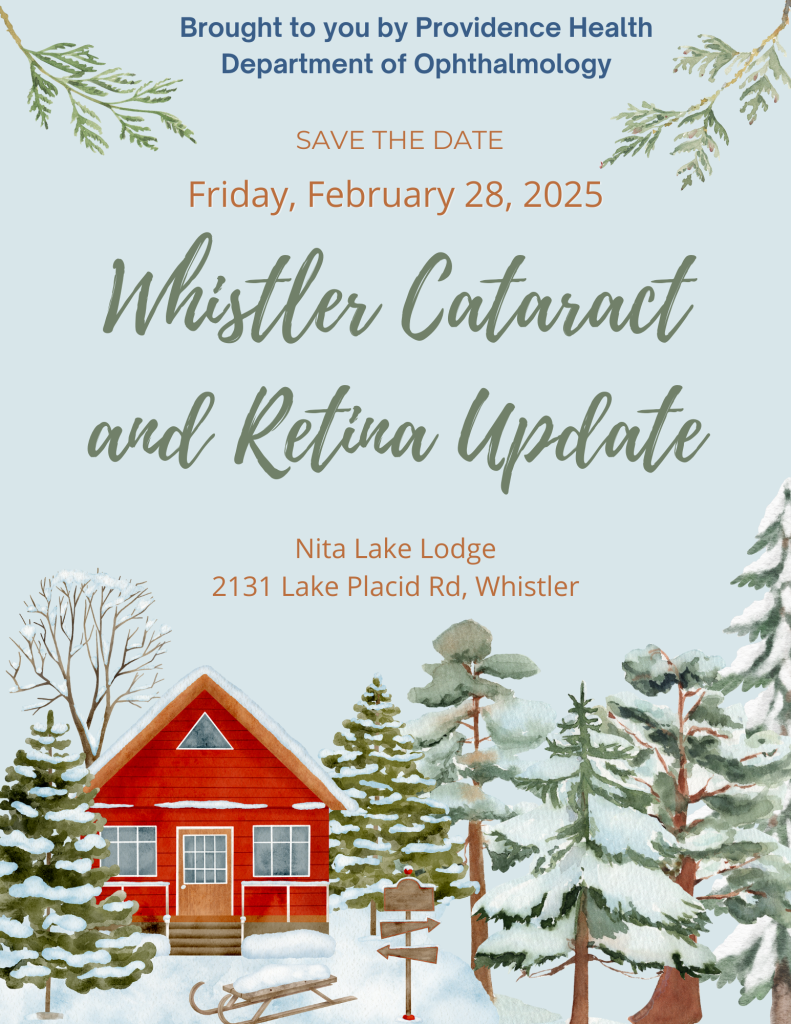
The Providence Health Department of Ophthalmology is pleased to announce that they will be hosting an in-person event called: Whistler Cataract and Retina Update: Innovations and Insights.
This one day event will bring together specialists for a day of learning with a focus on the integration of advanced IOL technologies in retina care to enhance surgical and patient outcomes.
When: Friday, February 28, 2025
Time: 8AM-4PM
Conference Location
Nita Lake Lodge
2131 Lake Placid Rd
Whistler, BC V8E 0B2
Directions/Map
Registration to this event includes: Course materials, welcome breakfast, lunch, refreshments and more!
Interested in registering? Click HERE for more information!
Tuesdays with the Titans: Ophthalmology Update & Review Lecture Series
The University of Alberta and ACUPO are eager to present: Tuesdays with the Titans: Ophthalmology Update and Review Lecture Series. This is a series of webinars that will be hosted on Tuesday evenings from 5:30 – 7:30 PM, MST. Learners are expected to:
- Apply the latest updates in comprehensive ophthalmology
- Review the 10 ophthalmic subspecialties prior to OKAP and the Royal College written exams.
The schedule is as follows:
| Date | Speaker | Topic | University |
| January 7th, 2025 | Alex Kaplan | Uveitis | University of Toronto |
| January 14th, 2025 | Michel Belliveau | Oculoplastics | University of Ottawa, Queens University |
| January 21st, 2025 | Ike Ahmed | Cataract | University of Toronto, University of Utah |
| January 28th, 2025 | Kamiar Mireskandari and Crystal Cheung | Pediatrics | University of Toronto |
| February 4th, 2025 | James Farmer | Pathology | University of Ottawa, Queens University |
| February 11th, 2025 | Delan Jinapraya | Glaucoma | Queens University |
| February 18th, 2025 | Hall Chew | Cornea | University of British Columbia |
| February 25th, 2025 | Paul Grewal | Retina | University of Alberta |
| March 4th, 2025 | Rahul Sharma and Claire Sheldon | Neuro-Ophthalmology | University of Toronto, University of British Columbia |
| March 11th, 2025 | Michael Wan | Optics | University of Toronto |
These webinars are eligible for MOC Section 1 Credits. Please contact [email protected] for registration information.
Maximize Your MOC Credits

To ensure you make the most of your learning activities, the Canadian Ophthalmological Society has curated some resources to help you maximize your MOC credits.
Discover how to make the most of your CPD activities and maximize your MOC credits throughout the year. This interactive mini-module guides you through a practical case study featuring Dr. Smith, who demonstrates how to turn diverse learning activities into optimal credit opportunities.
For the best user experience, we recommend accessing the course on a computer using a web browser. However, the module can still be accessed on a mobile device.
Joint Position Statement on the Use of Patented Microcurrent Technology for Dry AMD
The Canadian Ophthalmological Society (COS) and Canadian Retina Society (CRS) advise caution when considering a new microcurrent treatment for dry age-related macular degeneration (AMD). While early studies suggest it may help, there isn’t enough long-term evidence to confirm its safety or effectiveness. Retinal specialists, given their extensive expertise in managing age-related macular degeneration, recommend that patients and doctors discuss the treatment carefully and understand its limitations before deciding. The joint position statement is available to read below:
Diabetes Awareness Month
November is Diabetes Awareness Month, a time to highlight the critical role ophthalmologists play in managing diabetic eye disease. To support your practice, the Practice Resource Centre has compiled a curated list of insightful journal articles, clinical guidelines, and patient resources focused on diabetic retinopathy and related complications. Explore these valuable tools to stay informed and enhance patient care.
For Guidelines:
Diabetes Canada – Diabetic Retinopathy Guidelines
American Academy of Ophthalmology – Guidelines on Diabetic Eye Care
For Articles:
Retinal Physician – The Evolution of Clinical Trial Endpoints for Diabetic Retinopathy
JMIR Diabetes – Implementation of Artificial Intelligence–Based Diabetic Retinopathy Screening in a Tertiary Care Hospital in Quebec: Prospective Validation Study
Canadian Journal of Ophthalmology – Spectral-domain OCT characteristics of intraretinal hyper-reflective foci associated with age-related macular degeneration and diabetic retinopathy
Canadian Journal of Ophthalmology – Long-term visual outcomes and fluid compartment changes in limited-early versus early response to anti-VEGF treatment for diabetic macular edema
Canadian Journal of Ophthalmology – https://www.canadianjournalofophthalmology.ca/article/S0008-4182(24)00173-X/abstract
For Consensus Statements:
Ophthalmology and Therapy – Diabetic Disease of the Eye in Canada: Consensus Statements from a Retina Specialist Working Group
For Correspondence:
Canadian Journal of Ophthalmology – Acute bilateral diabetic papillopathy in a child



