RSA Course on Refractive Lens and Cataract Surgery
Date: July 3 – 6, 2024
Location: McGill University Health Center, 1001 Decarie Blvd, Montreal, Quebec
Registration is now open for the Refractive Surgery Alliance’s course on Refractive Lens and Cataract Surgery. This course is a comprehensive, interactive course that covers all aspects of refractive lens and cataract surgery and is open to all cataract and refractive surgery ophthalmologists.
The course covers the following key topics:
- Principles and philosophy of lens refractive surgery
- Lens-based approaches for the surgical management of presbyopia
- Patient evaluation and education
- Preoperative technologies, biometry, and surgical planning
- IOL technologies
- Surgical pearls
- Postoperative considerations and complication management
- Phakic IOLs and myopic lens surgery
- Growing your lens refractive practice
- Future considerations
The course faculty includes:
- Guillermo Rocha, MD, FWCRS (Course Chairman)
- Roger Zaldlvar, MD, MBA, FWCRS
- Samuel Masket, MD
- Damien Gatinel, MD, PhD, FWCRS
- Baseer Khan, MD
- Paul Harasymowycz, MD
- Guy M Kezirian, MD, MBA, FWCRS
- Erik Mertens, MD, FWCRS
To learn more about this course and for registration details, visit: https://www.refractivealliance.com/moderncataractsurgery/
Solar Eclipse Safety – Q&A

UPDATE (2024-04-17): We are collecting case reports on solar retinopathy following the recent solar eclipse. If a patient you’ve seen experienced vision impairment or related symptoms after viewing the eclipse, please fill out the following form to contribute to our research efforts. Your participation is crucial in helping us gather valuable data to better understand and mitigate the effects of solar retinopathy. You can access the form by clicking HERE.
Looking directly at the sun without proper protection can cause significant damage to your eye leading to a condition called solar retinopathy. During unshielded observation of a solar eclipse, the lens of the eye acts just like a magnifying glass, focusing the sun’s rays onto the retina at the back of the eye. This concentrated energy can result in permanent burns of the retina, and even irreversible blind spots.
The retina has no pain receptors. Therefore, it can take time before someone realizes that retinal damage may have occurred. You should be attentive to signs such as a blurry vision, visual distortion, and decreased colour vision and if you have looked at the solar eclipse without eye protection.
Let’s delve into some commonly asked questions about solar retinopathy and solar eclipse safety, and expert answers to equip both patients and providers with valuable insight during this event.
Commonly asked questions and answers
Q: What is the best primary prevention?
A: Refraining from viewing the solar eclipse is the best primary prevention to solar retinopathy. You can safely view the event indirectly, by TV or web.
Q: Which glasses are unsafe?
A: Sunglasses, glasses with transition lenses, glasses with polarizing filters, exposed film, x-ray film, and neutral density filters, do not provide enough safety to view the eclipse.
It is equally unsafe to view the eclipse from your telescope, camera, binoculars without the appropriate special filter, or through a window without the correct eye protection.
Q: Can one take pictures of the eclipse with a smartphone?
A: You can take pictures of the eclipse with your smartphone or tablet device, but make sure that you are not viewing the eclipse without the proper eye protection while aligning the device for the photo. Please keep in mind that some manufacturers state that prolonged pointing of the smartphone/camera to the sun may affect its sensors.
Q: What is the right filter to have when viewing the eclipse?
A: ISO 12312-2 certified. Upon receiving your glasses, please take the time to inspect as the glasses should not be scratched or torn. If the glasses are being worn by children, ensure that they are supervised at all times.
Q: What is the maximum duration of time that we can view the solar eclipse without permanent damage? What if I glance at the eclipse, look away, and then back again?
A: There is no duration of time that you can view the eclipse without permanent damage! The effects of the damage by the sun are cumulative, so looking at the eclipse multiple times would do more damage than looking at it once. It is advised that you do not look directly at the sun at all.
Please keep in mind that if on the totality path, to use great caution and under expert supervision to indicate the time that you may securely remove and put back on the certified glasses.
Q: Can animals suffer from solar retinopathy as well?
A: In theory, yes, if they are looking at the sun during the eclipse.
Q: Can someone with a previous history of ocular disease view the eclipse?
A: Yes, but only with precaution and the correct eye protection. If unsure, they can enjoy the solar eclipse by viewing it indirectly (such as through a livestream or broadcast on TV).
Resources
The authors of this Q&A on solar eclipse eye safety have compiled a comprehensive set of resources tailored to both patients and ophthalmologists, ensuring that everyone can access reliable information and guidance.
For the general public
Government of Canada – Stay safe while watching the solar eclipse
American Astronomical Society – Viewing the solar eclipse safely
Exploratorium – View the eclipse safely through livestream
Association des médecins ophthalmologistes du Québec – Éclipse solaire du 8 avril (French only)
Canadian Ophthalmological Society – Protect your vision
The Dose – How can I watch a solar eclipse and keep my eyes safe?
For the ophthalmologist
American Academy of Ophthalmology EyeWiki – Solar retinopathy
The Astronomical Journal – Physical and visual evaluation of filters for direct observation of the sun and the international standard ISO
Queen’s University – Grand Rounds Presentation: Total solar eclipse and eye health
Ophthalmology Times – Protecting vision during solar eclipses: Insights for ophthalmologists
Thank you to Dr. Marie-Josée Aubin and Dr. Cynthia Qian for creating this helpful resource!
Eyes on Oncology – Navigating corneal adverse events associated with antibody drug conjugates in oncology
The Master Clinician Alliance (MCA) is providing a Section 3 accredited online self-assessment program focusing on ocular AE assessment and management. Navigate through a learning path that includes a pre- and post-questionnaire, patients cases, knowledge questions as well as presentations.
QUICK AND EASY PARTICIPATION, NO ZOOM MEETINGS! Simply complete the program on your own, conveniently from your mobile device or computer. The program is expected to take about 1 hour to complete. Please note that the program is available in English and French.
Learning objectives:
By the end of this learning session, you will be able to:
- Describe the mechanisms of action and design of antibody drug conjugates (ADCs)
- Recognize the corneal toxicities caused by ADCs and propose appropriate corneal adverse event (AE) management strategies to minimize ocular complications
- Implement effective communication and coordination strategies to enhance collaborative care for oncology patients experiencing corneal toxicities
To register for this self-assessment program, please click HERE.
Canadian Eye Care Today: Volume 3, Issue 1
The latest issue of Canadian Eye Care Today is now available! This publication features clinical perspectives and practical information on topics in eye care relevant to today’s clinician. Its peer-reviewed articles focus on the treatment and management of eye disease from a Canadian perspective.
The content of this issue includes:
- Gene Therapy Updates for Inherited Retinal Dystrophies
- Melissa Lu, MD; Daniel Milad, MD; Cynthia X. Qian, MD, FRCSC.
- Recent Advances in the Evaluation and Treatment of Primary Angle Closure Disease
- Alanna James, MD; Benjamin Y. Xu, MD, PhD.
- Corneal Lumps and Bumps
- Mohammad Al-Fayyadh, MD; Mona Koaik, MD.
- Retinal Artery Occlusion and Neurovascular Risk
- Jesia Hasan, MD, FRCSC.
- Approach to Infectious Keratitis: Clinical Pearls While on Call
- Sonia N. Yeung, MD, PhD, FRCSC, FACS; Alfonso Iovieno, MD, PhD, FRCSC, FACS; Barbara Burgos-Blasco, MD, PhD.
To access the latest issue, click on the picture below!
CJO: February 2024 Issue Highlights

The February 2024 CJO is now available online. Here are some of the highlights:
Editor-in-Chief’s report: 2023 at CJO: In this editorial, Dr. Varun Chaudhary highlights some of the CJO’s key accomplishments and outcome metrics from 2023, including another significant increase in the journal’s Impact Factor, which now sits at 4.2.
Resident Perspectives + visual abstract: Our talented team of residents have summarized 3 articles with a focus on what’s most relevant to ophthalmology learners here in Canada and around the globe. In addition, our February visual abstract provides a visual summary of an article on Risk factors for ischemic cerebral stroke in patients with acute amaurosis fugax.
Original research articles:
- Analysis of ophthalmology subspeciality opioid prescribing patterns during the opioid public health crisis
- Safety and efficacy of micropulse transscleral cyclophotocoagulation
- Use of virtual care in ophthalmology in Ontario, Canada in 2020 during the COVID-19 pandemic
- Equity, diversity, and inclusion landscape in Canadian postgraduate medical education for ophthalmology
- Multifocal electroretinographic findings in angiographic macular leakage in the setting of intermediate, posterior, or panuveitis
Research letters, photo essays, and case reports:
- Comparison of ChatGPT to ophthalmology resident and staff consultants on an ophthalmological training tool [research letter]
- Text-to-image artificial intelligence models for preoperative counselling in oculoplastics [research letter]
- Cilioretinal artery occlusion secondary to central retinal vein occlusion [photo essay]
- Retinal ischemic perivascular lesions and sickle cell maculopathy [photo essay]
- Strabismus in early disseminated Lyme disease: case report and summary of the literature [case report]
- Poor response of solitary optic disc retinal capillary hemangioblastoma to intravitreal propranolol [case report]
- Blockchain technology: revolutionizing ophthalmology and patient-centered care [correspondence]
Follow the CJO on social media:
Facebook: CanJOphth
Instagram: @cjo_jco
LinkedIn: CJO – JCO
Twitter: @CanJOphth
COS Forum 2024 – Exploring the Future of Ophthalmology
Thank you to all the participants who were able to join us during the live session, we hope you enjoyed the webinar! We are pleased to offer a recording of the forum. If you missed the live session, you will still be able to access presentations on Advocacy; Artificial Intelligence; Sustainability in Ophthalmology; and Drug Shortages & Essential Medications.
Learning objectives:
- Understand how COS is advocating for policy changes at the government level to improve eye care accessibility and quality
- Be able to describe how COS is working with partners at Health Canada to analyze the causes and consequences of ophthalmic drug shortages and develop strategies to lessen their impact on patient care
- Know more of the current and potential applications of artificial intelligence (AI) in ophthalmology and their potential to impact patient care and clinical decision-making
- Be more aware of the environmental impact of ophthalmic practices and devices and the strategies for promoting sustainability in ophthalmic practice
IV Issue – 2023 Video Journal of Cataract, Refractive, & Glaucoma Cases

The fourth issue of the 2023 Video Journal of Cataract, Refractive & Glaucoma Surgery is out! This issue is titled: SHOCKING CASES!
The Video Journal of Cataract, Refractive and Glaucoma Surgery (VJCRGS) represents a lifelong mission of renowned ophthalmic surgeon and educator, Robert H. Osher, MD, to advance knowledge and surgical training of eye surgeons. The VJCRGS pioneered video-based surgical education when it debuted in 1985 as a quarterly subscription serving the needs of cataract and refractive surgeons. In 2018, the Video Journal’s scope expanded to include glaucoma surgery in line with the evolving trends in anterior segment surgical management.
Table of contents
| The Quest | Dr. Robert Osher, USA |
| Descemet Detachment | Drs. Vineet Ratra, Bhaskar Srinivasan & Dhanashree Ratra, India |
| Intrastromal IOL Injection | Drs. Roopashree Matada, Praveen Murthy, & Vinay R Murthy, India |
| Nightmare During Suture Removal | Drs. Blanca Sanz-Magallon, Aamir Ismailjee, & Alfonso Vasquez-Perez, UK |
| Volcano! | Drs. Lionel Raj Daniel Ponniah, Heber Anandan, & Mohamed Ali, India |
| Black Add On IOL | Drs. Volker Besgen & W. Sekundo, Germany |
| Mega Implantable Contact Lens | Drs. Jagat Ram, Parul Chawla Gupta, Simar Rajan Singh, Vijay Sharma, Bala Murugan, Surbhi Khurana, Amit Gupta, & Sushmita Kaushik, India |
| Capsular Bag Transplantation | Dr. Yuriy Kondratenko, Ukraine |
| IOL Optic Transplant | Drs. Fernando Gonzalez Del Valle, Maria Jose Dominquez Fernandez, Javier Celis Sanchez, Antonio Arias Palomero, Jose Juan Valdes Gonzalez, Laura Riviera Villalobos, Edgar Infantes Molina, & Laura Garcia-Filoso Moraleda, Spain |
| Staphyloma | Drs. Sonam Yangzes, Chintan Malhotra, A K Jain, & Amit Gupta, India |
| Two Keratoprostheses | Drs. P. Stodulka & A. Mackova, Czech Republic |
To access this educational content, visit: http://www.vjcrgs.com/
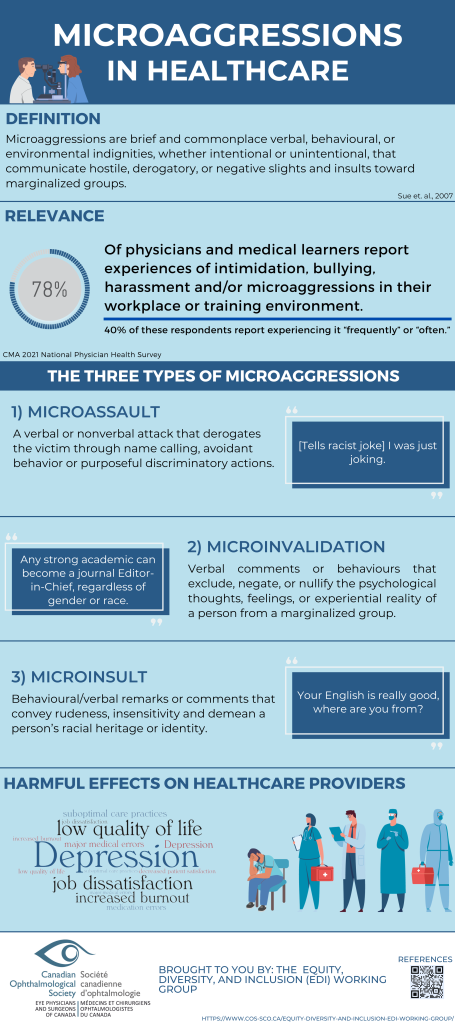
Equity, Diversity and Inclusion (EDI) Toolkit
We recognize the importance of promoting a more inclusive and diverse community of ophthalmologists, and we’re committed to providing valuable resources to support our members in this journey including a glossary of EDI terms, online resources, and infographics.
By embracing EDI principles, we can create a more equitable and welcoming environment for patients and professionals alike. As you engage with our resources, remember that embracing these principles not only benefits your own professional development but also enhances the quality of patient care.
We invite you to actively participate in promoting EDI within ophthalmology. Share your insights, experiences, and suggestions to help us expand our resources and support for the community.
Glossary of EDI Terms: Understanding the language of EDI is an essential first step in promoting inclusivity and diversity within your practice. Explore our short glossary of key EDI terms.
LEARN MORE
Incorporating EDI Principles into Your Organization or Team: Learn how to foster an inclusive environment by understanding and implementing Equity, Diversity, and Inclusion principles.
LEARN MORE
Anti-Racism: Discover strategies and resources for addressing and combating racism within your organization or team.
LEARN MORE
Implicit Bias: Explore the impact of unconscious bias and ways to mitigate its effects in your workplace.
LEARN MORE
Microaggressions in Healthcare: Recognize and address microaggressions that occur in healthcare settings, fostering a more respectful environment.
LEARN MORE
Strategies to Approach Microaggressions: Gain practical techniques and insights for effectively addressing and reducing microaggressions in your organization.
LEARN MORE
Resources for Conducting Research: Access tools and references for conducting research that promotes Equity, Diversity, and Inclusion in your field.
LEARN MORE
Resources for Medical Education and Residency: Discover educational resources and strategies for integrating EDI principles into medical education.
LEARN MORE
Economics & EDI: Explore the economic aspects of Equity, Diversity, and Inclusion, and how they impact your organization or team.
LEARN MORE
Videos and TED Talks: Access a collection of insightful videos and TED Talks that provide valuable perspectives and practical insights on Equity, Diversity, and Inclusion.
LEARN MORE
Other Resources on Equity, Diversity, and Inclusion:
Find additional valuable resources to deepen your understanding and implementation of EDI principles beyond the listed categories.
LEARN MORE


CJO: December 2023 Issue Highlights

The December 2023 CJO is now available online. Here are some of the highlights:
Resident Perspectives + visual abstract: Our talented team of residents have summarized 4 articles with a focus on what’s most relevant to ophthalmology learners here in Canada and around the globe, including the article featured in our October visual abstract, Comparison of pre-formalin fixation and postfixation temporal artery biopsy lengths
Original research articles:
- Updated inventory and projections for Canada’s ophthalmology workforce
- Long-term outcomes of type 1 retinopathy of prematurity following monotherapy with bevacizumab: a Canadian experience
- Assessment of the optic nerve, macular, and retinal vascular effects of COVID-19
- Idiopathic epiretinal membranes: postoperative changes in morphology
- Impact of inherited retinal diseases on Canadian patients and families: a mixed-methods study
- Backlog in ophthalmic surgeries associated with the COVID-19 pandemic in Ontario 2020
Research letters, photo essays, and case reports:
- Antibiotic resistance profile in bacterial keratitis: a single-centre study [research letter]
- Costs associated with treating uveal melanoma are understudied [research letter]
- Hyperviscosity retinopathy from chronic myelogenous leukemia [photo essay]
- Diffuse infiltrating retinoblastoma: a panuveitis masquerade [photo essay]
- Variable phenotypic expression of MYOC mutations in a family with inherited pediatric glaucoma [case report]
- Rapidly progressive optic neuropathy due to optic nerve sheath meningioma following hormonal fertility treatment [case report]
- Optical coherence tomography angular hyperreflectivity as an early sign in acute macular neuroretinopathy [case report]
Follow the CJO on social media:
Facebook: CanJOphth
Instagram: @cjo_jco
LinkedIn: CJO – JCO
Twitter: @CanJOphth




